One of the long-standing unanswered questions in medical science is the role of the mind in physical health.
A well-known example is the placebo effect, the reduction or elimination of symptoms in an ill person from taking a "medicine" with no active ingredients. Less known, but also well documented, is the nocebo effect, where someone believes they will come to harm, often from supernatural means -- as in voodoo curses -- and then actually does. (Placebo and nocebo come from Latin, and mean "I will please" and "I will harm," respectively.)
The mechanism by which this could occur is poorly understood at best. We do know that in situations of high emotional or mental stress, the body produces hormones like adrenaline and cortisol, which can have long-term deleterious effects (thus the connection between stress and inflammatory diseases), but it seems like there must be more to it than that.
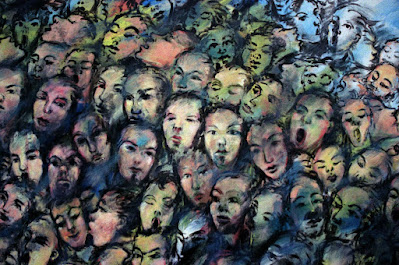
And that's not even as complicated as it gets. Consider, for example, folie à deux -- also called shared psychosis -- when two people experience the same strange delusions. How this happens and the mechanism by which it works are unknown, and the results can be nothing short of bizarre.
The best example I've ever heard of folie à deux is the case of June and Jennifer Gibbons. The two were identical twins, born in 1963 in Yemen to British subjects originally from Barbados. By 1974 the girls, their parents, and three other (completely normal) siblings were living in Haverfordwest, Wales, where their father worked as a Royal Air Force technician and their mother was a homemaker.
The twins started exhibiting odd behavior as toddlers. They rarely spoke except to each other, and their conversations were conducted in a largely invented language based in part on a sped-up version of Bajan Creole. (Siblings inventing their own private language isn't that uncommon, and is called idioglossia; but here, the twins seemed entirely unwilling to speak in English, nor to anyone but each other.)
The parents, and the girls' teachers, tried everything they could think of to break this strange link. Sending them to separate boarding schools completely backfired; both girls became catatonic, refusing to eat or move until they were reunited. The one way they would let anyone else know what was happening in their minds was through writing. Given a gift of diaries when they were sixteen years old, they began writing elaborate stories -- but filled with violence and disturbing imagery.
In 1981, following a string of petty crimes they were accused of, the twins were committed to Broadmoor Hospital, where they were eventually to spend twelve years. And this is where things took an even more peculiar turn, because they told the staff at Broadmoor that the only way one of them would live a normal life is if the other died. It didn't matter which; to break the spell required one of them to die, after which the other would go on to speak, act, and live normally.
In 1993, they were transferred to Caswell Clinic in Bridgend, Wales, and upon arrival, Jennifer was found to be unresponsive. She was admitted to the hospital where she lingered, comatose, for a week, but finally died due to what an autopsy found to be acute myocarditis (inflammation of the heart). Strangest of all, there were no drugs, poisons, or infectious agents in her system that could be found to explain the illness, and the inquest ended with a finding of "ultimate cause of death unknown."
A week after her sister's death, June told a therapist, "I'm free at last, liberated, and at last Jennifer has given up her life for me," and described the moment of Jennifer's death as hitting her "like a tsunami." She was monitored by psychiatric services for several years, but eventually was discharged, because -- exactly as the sisters had predicted -- the survivor had begun living an entirely normal life. By 2008 June had a flat near her parents in a small village in western Wales, and was working and socializing like any ordinary person would.
What on earth could have caused this bizarre situation?
The simple answer is "we have no idea." There is nothing in what is known of the Gibbons family's background that could account for it; judging by statements from the twins' siblings, they seem to have been a completely ordinary working-class family. Strangest of all is the circumstances that severed the connection between Jennifer and June. Did Jennifer Gibbons actually "will herself to die" to free her sister, or was there something more sinister going on? What was the nature of the link between them -- and how can we account for the medical and psychological manifestations of it?
Once again, there are no clear answers. We're left with more questions -- particularly, how the mind creates the world of perception we live in, and how it can go so drastically wrong for certain unfortunate people. The treatment of psychiatric illness is certainly far better than it was even forty years ago, when the Gibbons twins started their decade of life in Broadmoor, but we're still largely in the dark about how the mind works -- and how it can so profoundly affect the body in which it resides.
****************************************
 |